Improving Chronic Pain Management by Reducing Harm from Opioids
Our ambition is to reduce harm from opioid medicines by reducing high-risk opioid prescribing by 50% by March 2024.
There is no evidence for efficacy of high dose opioids (>120mg/day morphine equivalent) in long term pain. The Faculty of Pain Medicine has advised that increasing opioid load above this dose is unlikely to yield further benefits but exposes the patient to increased harm https://www.bma.org.uk/media/2100/analgesics-chronic-pain.pdf
Despite this, PHE’s review (2019) shows that in 2017 to 2018, 540,000 adults in England were prescribed opioid pain medicines for 3 years or more Prescribed medicines review: report – GOV.UK (www.gov.uk)
The effects of COVID-19 are anticipated to have exacerbated the use of opioids for chronic pain which is linked to both deprivation and the prevalence of mental health conditions such as anxiety.
A diagnostic exercise was undertaken based on an analysis of published literature and real-world case studies from across England, submitted by the regional AHSNs. The full report can be accessed here Improving-Chronic-Pain-Management-by-Reducing-Harm-from-Opioids-Report_2021
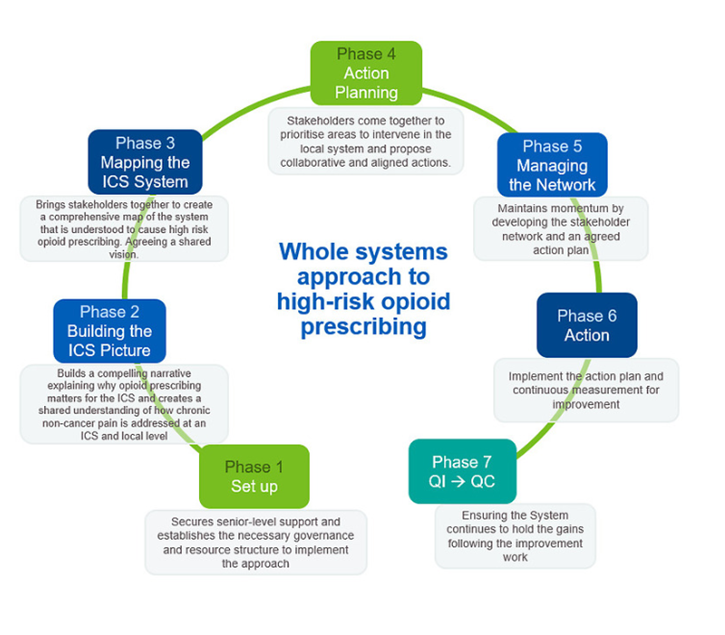
Based on this work, the AHSN network has developed a whole systems approach to reducing harm from opioids to support local approaches to helping people live well with chronic non-cancer pain; the detail of this plus supporting background information can be accessed through NHS Futures
NHS Futures: Whole systems approach to high-risk opioid prescribing (registration is required for access to NHS Futures).
We are working with colleagues in the Frimley Health and Care Integrated Care System (ICS) to define, develop and deliver this whole system programme which improves the care required to assist people to ‘live well with pain’. We are currently at Phase 2 of the Whole System Approach, using data from the ePACT2 national opioid dashboard to build a picture of prescribing within the ICS. https://www.nhsbsa.nhs.uk/access-our-data-products/epact2 .